Sun, 26 June 2016
We cover a Scancrit post on the Back Up Head Elevated (BUHE) intubation position. This post details a multicenter retrospective observational study by Khandelwal et al in Anesthesia & Analgesia. Intubating with the head elevated (ear to sternal notch) and the back of the bed up reduces complications. We delve into core content on the esophagus using Rosen’s (8th ed) Chapter 71 and Chapter 77 in Tintinalli (8th ed). We discuss dysphagia, food impaction, and esophagitis.
JEremy Faust and Lauren WEstafer
Direct download: Foamcast_52_Back_up_head_elevated_intubation_-_6-25-16_5.17_PM.mp3
Category:general -- posted at: 8:56am EDT |
Thu, 16 June 2016
We cover pearls from smaccDUB (Social Media and Critical Care Conference in Dublin, Ireland), Day 3. We are here thanks to the Rosh Review. Dr. Scott Weingart - "Post-Intubation Sedation"
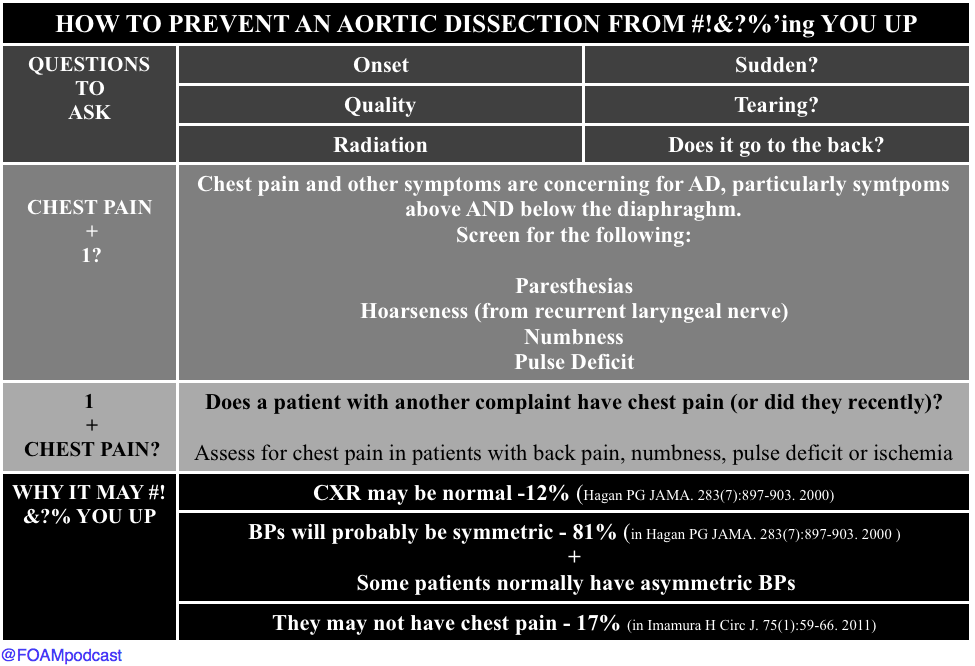
Dr. David Carr - "The Aorta Will #!&?% You Up" Dr. Kathleen Thomas - "Oh Sh**! They’re bombing the hospital!" We should not need a website entitled STOPBOMBINGHOSPITALS.ORG but, unfortunately, over the past 4 years, 400 hospitals have been bombed. This passionate, wrenching talk is a "must see" and "must listen" when the free talks are released on the SMACC podcast over the course of the next year. ive use in the emergency department. Emergency medicine journal : EMJ. 30(11):893-5. 2013. [pubmed]
Direct download: Foamcastini_smaccdub_day_3_aorta_and_pain.mp3
Category:general -- posted at: 2:01pm EDT |
Wed, 15 June 2016
#smaccDUB day 2 Dr. Reuben Strayer - “Disruption, Danger, and Droperidol: Emergency Management of the Agitated Patient." Dr. Strayer presented a brilliant talk on dealing with the quintessential Emergency Medicine patient - the undifferentiated acutely agitated patient. These patients are high risk and require emergent stabilization and resuscitation. Dr. Haney Mallemat - "The PEA Paradox" The typical way we think about PEA, the "H's and T's," is overly complicated. Further, we are horrendous at pulse palpation (see this for more), and so what we think is PEA may not actually be PEA. Dr. Mallemat proposed QRS duration as one way to think about PEA, although this has limitations. Dr. Michele Dominico - "How Usual Resuscitative Maneuvers Can Kill Paediatric Cardiac Patients" Interventions we jump to in sick patients - oxygenation, ventilation, vasopressors - these can kill pediatric patients with cardiac pathology. She gave examples of some high yield pearls in these already terrifying patients. EM Literature update by Drs. Ashley Shreves and Ryan Radecki
Interesting and Ridiculous Research Pearls from Drs. Ashley Shreves and Ryan Radecki
|
Tue, 14 June 2016
We are at SMACC in Dublin - thanks to the Rosh Review, an excellent board review question bank. Here are some of our favorite pearls. Do We Make Saves? Dr. Mervyn Singer "Is Survival Predetermined in the Critically Ill?"
Favorite Pearls Dr. Suzanne Mason - "Acute Care of the Elderly"
Dr. Victoria Brazil - "So You Think You're a Resuscitationist?"
Direct download: FOAMcastini_SmaccDub_Saves_day_1_-_6_14_16_7.56_PM.mp3
Category:general -- posted at: 3:05pm EDT |
Thu, 9 June 2016
We cover this short video from EMRAP on lateral canthotomies. This is one of those rare procedures that is vision saving; hence, it is worthy of frequent review. Then, we delve into core content on orbital fractures, hyphemas, and ocular burns using Tintinalli and Rosen's Emergency Medicine as a guide. Show notes and references at foamcast.org Thanks for listening! Jeremy Faust and Lauren Westafer |
FOAMcast - An Emergency Medicine Podcast

Categories
generalmedicine, urology, emergency medicine
medicine, emergency medicine, toxicology, foam, emergency medicine resident
transfusions
medicine, psychiatry, ICP, emergency medicine
emergency medicine, foam, hepatic emergencies
acid-base
electrolytes
pregnancy
infectious disease
allergy
toxicology
cardiology
neurology
trauma, spleen
conferences, FOAM, smacc
environmental, emergency medicine
medicine, cardiology, toxicology, emergency medicine
ortho
statistics
emergency medicine, neurology
respiratory
gastroenterology
Archives
FebruaryDecember
October
September
March
February
January
December
October
September
July
June
March
January
December
November
October
September
August
July
June
April
March
February
January
December
November
October
September
August
July
June
May
April
March
February
January
December
October
September
July
May
April
March
February
January
December
November
October
September
August
July
June
May
April
March
February
January
December
November
October
September
August
July
June
May
April
March
February
January
December
November
October
September
August
July
June
May
April
March
February
January
December
November
October
September
August
July
June
May
April
March
February
January
December
November
October
September
August
July
June
May
| S | M | T | W | T | F | S |
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||
| 5 | 6 | 7 | 8 | 9 | 10 | 11 |
| 12 | 13 | 14 | 15 | 16 | 17 | 18 |
| 19 | 20 | 21 | 22 | 23 | 24 | 25 |
| 26 | 27 | 28 | 29 | 30 | ||
Syndication